I am happy to be blogging this post from the comfort of home! Don't ever try to blog on an iPad. If happened to be following along and noticed typos and things changing around yes, that happened. Every time I tried to scroll the iPad wouldn't allow me to like the keyboard froze, so to get to the part of the post I was writing I had to hit return multiple times until it got to the bottom and then go and delete all the returns. It would bump me back up to the top and the process would repeat. It was nearly as painful as our week at the hospital. But I know some of our family was watching for updates. That might include some members of my sorority sisters, those trach moms who know all too well the experience of hospitalization and/or surgery with their child. Many of those people really are interested in the medical details, but if that bores you then feel free to skim.
*****
We had a decent night's sleep after the night nurse was able to better arrange our meds so that they only had to wake her twice instead of 5 times (I made a bit of a fuss). Sleep is more important than following a rigid med schedule. This is what we came home with.
It's important to stay on top of the post-operative pain. In my opinion it's best to keep on the narcotics for the first week and continue alternating the harmless tylenol and ibuprofen. She started to have headaches. I'm not sure if it was from the epidural or from when they didn't give her the oxycodone on schedule as I'd requested. They seemed to spike but have gone. I was pretty impressed that she was able to communicate it so clearly.
The downside to surgery and narcotics is that they can slow down your digestion which has been a big issue for Ainsley this time. Once she started eating she ate really well. Until a point when her stomach started to be too full. When she was transitioned to oral meds she had some gagging which has made it difficult. Toward the end she refused to open her mouth and even started covering it. In the morning I could barely get her to eat a bowl of Cheerios. Things have started to get better and I think her stomach will be back to normal soon.
We chose green with pink stripes. Ian did a great job carefully making the stripes. He was awesome.
They seemed to really enjoy Ainsley as a patient. Cute aren't they? Unfortunately they'll be mostly covered with the braces most of the time. She has to wear them nearly all day for the next 6 weeks.
One of the biggest issues for us is that Ainsley HATES having an IV. It was slightly better once it wasn't running any meds and was saline locked. But even then she kept asking for it to be removed.
Until it was time to remove it and then she screamed bloody murder.You can see how much trouble she has breathing when she cries. Notice the sunken trach stoma. Poor love.
After I removed the bandaid (they have to put one one because they bleed) she was happy. The nurse said she's NEVER seen anyone be so happy to get their IV out.
She kept showing me and others her brave doll, waving it around. I think it's her way of saying "I'm been brave." When I put Netflix on her iPad finally she was starting to be happy again.
But alas there is a lot of work to be done. We had to complete training. Due to the fact that they cut her heel bones and then grafted in donor bone and created an arch for her feet it is critical that she not bear ANY weight for the entire first 6 weeks. Not to use the bathroom, not to make transfers from bed to wheelchair, NOTHING.
So they made me simulate a transfer into a car in the hospital bathroom using the slide board. It is not easy. But I think we got an A+. Ainsley is stronger than she looks and they were amazed and how well she helps. I don't know how the parent of kids with more severe CP manage when the child can't help with their arms. I'm really lucky, but it's still hard on my back. Of course sleeping on an extra firm pull out couch exacerbates my already bad back. I'm glad to be back to a normal bed tonight! It is going to be a tough 6 weeks but will probably go by quite quickly.
A good part of the morning was taken up trying to get a commode since we aren't sure I will be able to get the wheelchair (it's big) up to our toilets to do a safe slide board transfer. They delivered the wrong thing: a commode with fixed arms that would be useful to us. Doesn't it figure?!
High fives for passing our PT lessons so we can discharge.
I requested some wedges to help with positioning. They came up with these special gel pack things that hold whatever form you put them in. They were AWESOME. I just wish they'd given them to us day one. I'm going to show the surgeon. We were using pillows which often ended up getting out of ideal position. After hamstring lengthening you want the weight of the legs to naturally straighten the leg as much as they can, without the heels touching the bed (to protect the calcaneal osteotomies). Using these will speed up the process of straightening her legs and prevent the muscles from going back to their old position.
One interesting development this hospitalization is that Ainsley learned to use the call button to get the nurses. By the end of this stay she had zero reservations about using it. But she would also buzz them nearly every time I left the room. We were lucky when we were moved to the floor that we were literally right next to the parent room. I could go get myself water or put food in the refrigerator in a couple minutes. But she still would call the nurses to ask where I was even though I told her.
Thankfully they've added room service for families. So I was able to order food to be delivered (usually when she ate) and not have to leave her. The cafeteria is quite a distance and in the past it wasn't common for me to skip meals because it was so hard to go get food. This is a great thing for patients: parents can eat with their child!
We got to finish watching Paddington Bear while waiting for Steve to show up. Our room was all packed up and we were READY!
Ainsley was very happy to see her daddy! She asked about him multiple times every day.
This time when we saw the elephant she was happy and gave the "halleluah" arms in the air.
Getting out and about is going to be difficult. Steve is able to lift her safely (for her) because he is tall. Even in his bigger vehicle it was a tight squeeze. I'm still borrowing my sister's car (for Evie too) which is a compact sedan and it's not going to be easy to get Ainsley's legs or the wheelchair in.
It felt so great to be driving away from the hospital. Even when traffic on Montlake was at a complete stop. It was so nice to see Mt. Rainier as we drove over the bridge.
As we were driving Ainsley used her AAC device to say "Evie, Adrian, foot" which I understood to mean she was excited to show Evie and Adrian the casts on her feet. I showed her how to say it fully. I found it quite interesting that she wanted me to know that was what she wanted. A pretty cool moment in communication for a genuine purpose other than requesting.
Evie, Adrian and Penny greeted her with high fives and tail wags (and a lot of excited barking of course).
We had promised Ainsley some time doing her favorite thing: playing Mario Brothers. She is allowed to be out of the braces for an hour twice a day during (part of which we will spend doing PT). Her positioning here isn't as good as it should be, but we cut her some slack after a very difficult week. She had so much fun and is so glad to be home!
I had a couple much needed beers by myself while I sat in my recliner and chose the pictures to upload for this post.
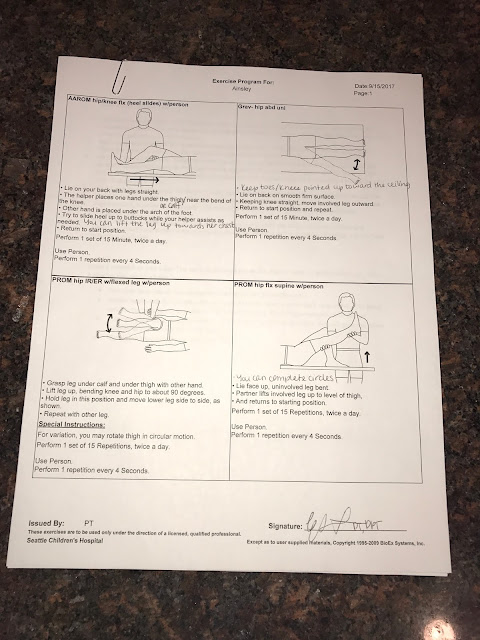
Then it was back to work teaching Steve the things I was taught during our stay, starting with the exercises we will be doing.
Steve has given up his spot in bed for Ainsley to have the comfort of sleeping next to mom in a comfy bed. Her breathing is still a bit labored but we are hoping for improvement over the next week. Having her in bed with me also makes it easier for me to keep an eye on her and also give night meds. I'll keep you all posted if there are any changes. No news is good news.





























































.JPG)
